Heart disease in women: Understanding gender-specific risk factors
By Christina Reuss, MD | HonorHealth Heart Care

Christina Reuss, MD
Heart disease is the leading cause of death for women in the U.S., causing one in three deaths each year. Nearly 45% of women aged 20 and older are living with some form of cardiovascular disease. Despite this, only 44% of women recognize that cardiovascular disease is their greatest health threat. [1] Cardiovascular disease kills more women than all forms of cancer combined. Physicians and APPs must understand the unique aspects of cardiovascular disease presentation and risk factors in women to ensure optimal patient care and outcomes.
Gender-specific risk factors
Women face several distinct cardiovascular risk factors that deserve special attention.
- Pregnancy complications, particularly preeclampsia and gestational diabetes, can increase heart disease by two to three times, significantly impacting long-term cardiovascular health.
- Hormonal changes during menopause, especially premature menopause, play a crucial role, as declining estrogen levels can negatively affect heart health.
- Polycystic ovary syndrome (PCOS) increases the risk of both heart disease and type 2 diabetes.
- Angina with normal coronary arteries (ANOCA) and spontaneous coronary artery dissection (SCAD) are conditions with higher prevalence in women:
- ANOCA, a heterogeneous condition with multiple mechanistic pathways, is best diagnosed using functional diagnostic angiography in addition to standard coronary angiography. There is a higher prevalence of non-obstructive coronary disease in women. [2]
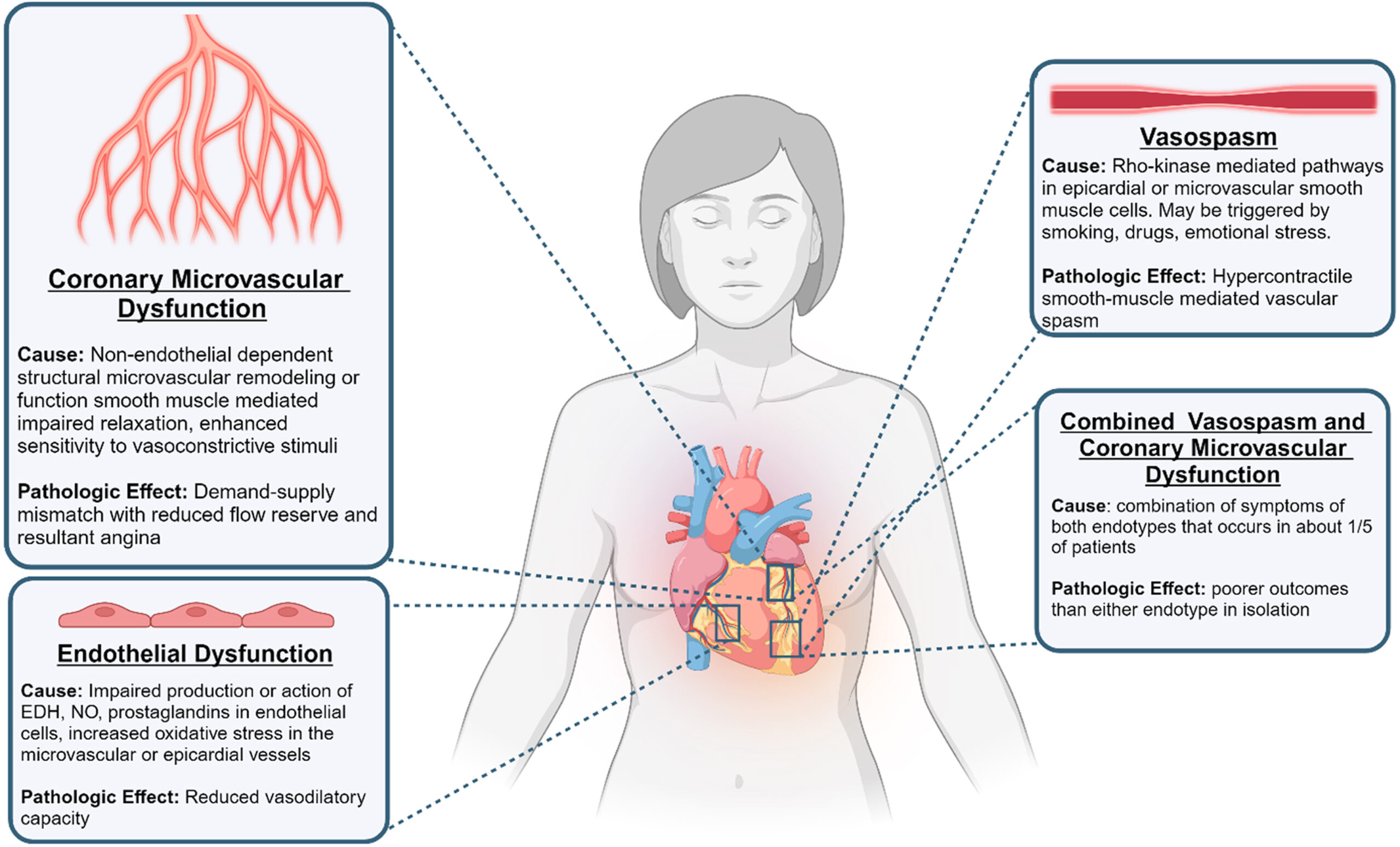
Figure 1: Pathophysiologic Endotypes of ANOCA. The four endotypes include: 1) coronary microvascular dysfunction; 2) endothelial dysfunction; 3) vasospasm; and 4) combined epicardial vasospasm and microvascular dysfunction.
- SCAD is an increasingly recognized cause of acute coronary syndrome, particularly in young women with few conventional cardiac risk factors.[3] It is associated with premenopausal women, pregnancy, high physical or emotional stress and has a strong correlation with fibromuscular dysplasia.
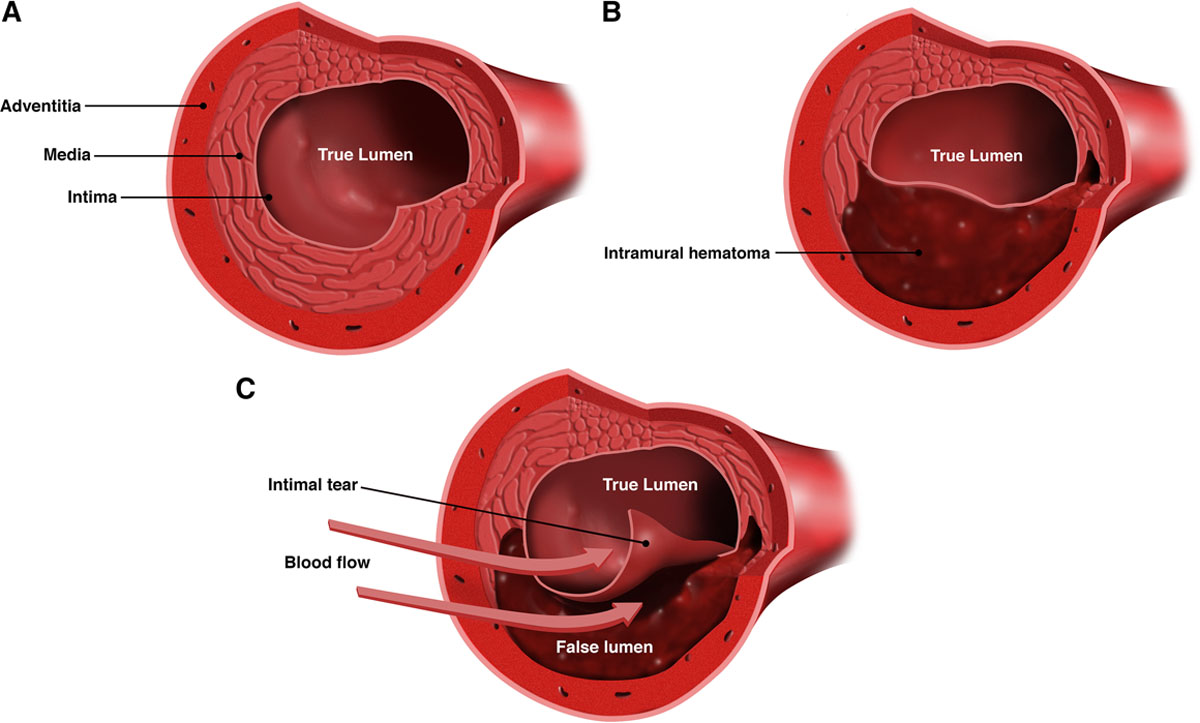
Figure 2: Spontaneous coronary artery dissection (SCAD) anatomy and presentation
Unique symptom presentation
Women often experience heart attack symptoms differently than men. While chest pain remains common, women are more likely to report:
- Unusual fatigue and sleep disturbances weeks before a cardiac event
- Shortness of breath and anxiety
- Pain in the jaw, neck or upper back
- Nausea and vomiting
- Lightheadedness or dizziness
These differences in symptom presentation can lead to delayed diagnosis and treatment. Data shows that 23% of females 45 years of age and older who had an initial myocardial infarction (MI) died within a year compared with 18% of males.[4] Within five years after a first MI, 47% of females died compared to 36% of males, highlighting the critical importance of early recognition.
Risk factors common to both genders
Traditional risk factors affect both men and women but may impact women differently:
- High blood pressure typically develops later in life for women but can be more severe. In fact, 51.9% of high blood pressure deaths are in women, with Black women having the highest prevalence (57.6%) of any race or ethnicity.[1]
- Diabetes increases heart disease risk more significantly in women than men, requiring careful management.
- Smoking has a proportionally greater negative impact on women’s heart health.
- Depression and stress, more common in women, contribute to increased cardiovascular risk.
Prevention and early detection
Less than 50% of women entering pregnancy have good heart health.[5] Additionally, 10-20% of women will have a health issue during pregnancy that can impact their long-term cardiovascular health. Medical professionals should implement gender-specific strategies for prevention and screening:
- Obtain detailed pregnancy histories during cardiovascular risk assessments (preeclampsia, gestational hypertension and gestational diabetes).
- Monitor blood pressure and metabolic health more frequently in postmenopausal women.
- Screen for depression and stress as part of routine cardiovascular care.
- Educate patients about women-specific symptoms and risk factors.
- Consider more aggressive prevention strategies in women with multiple risk factors.
Diagnostic considerations
Given these unique symptom presentations and risk factors, gender-specific challenges in cardiac diagnostics should be considered:
- Standard exercise stress tests may be less accurate in women, with higher false-positive rates.
- Single-photon emission computed tomography (SPECT) imaging can be affected by breast tissue attenuation, potentially leading to false-positive results.
- Coronary microvascular disease, more common in women, may not be detected traditional angiography. In these cases, clinicians should consider referring patients for functional angiography (offered at HonorHealth).
- Stress echocardiography, nuclear PET or cardiac MRI may provide better diagnostic accuracy in women and should be considered when appropriate.
Future directions
Research continues to reveal gender-specific aspects of heart disease. Emerging evidence suggests that men and women may benefit from different diagnostic and treatment approaches. Physicians and APPs should stay informed about the latest findings to provide optimal care for female patients.
By prioritizing gender-specific approaches to prevention, diagnosis and treatment, and emphasizing early recognition and intervention, we can significantly improve outcomes for female patients and reduce the devastating impact of this disease.
HonorHealth Women’s Heart Health Program
The HonorHealth Women’s Heart Health Program offers comprehensive cardiovascular care across all stages of a woman’s life. Our specialized expertise includes pregnancy-related cardiac care, prevention and management of cardiovascular conditions and gender-specific treatment approaches. Our multidisciplinary team provides evidence-based, integrative care plans tailored to each patient’s needs. To learn more, visit HonorHealth.com/WomensHeart.
References
American Heart Association. Facts About Heart Disease in Women. Go Red for Women. Published 2024. https://www.goredforwomen.org/en/about-heart-disease-in-women/facts
JACC Advances. 2024 Aug, 3 (8) 101074. https://www.jacc.org/journal/jacc-advances
Circulation. Volume 137, Number 19. https://doi.org/10.1161/CIR.0000000000000564
American Heart Association, Inc. 2022 Heart Disease & Stroke Statistical Update Fact Sheet.; 2022. https://www.heart.org/-/media/PHD-Files-2/Science-News/2/2022-Heart-and-Stroke-Stat-Update/2022-Stat-Update-factsheet-Females-and-CVD.pdf.
Research adds to knowledge about heart disease and stroke in women of all ages. American Heart Association. Published 2024. https://newsroom.heart.org/news/research-adds-to-knowledge-about-heart-disease-and-stroke-in-women-of-all-ages
